What is Continuous Glucose Monitoring and How Does It Work?
If you’ve been curious about how to keep a closer eye on your health without the hassle of constant finger pricks, let’s talk about continuous...
4 min read
 Dr Kaufman
:
May 26, 2025 2:06:32 PM
Dr Kaufman
:
May 26, 2025 2:06:32 PM

In the 21st century, medical science has given us incredible tools to understand our bodies. From genetic testing to advanced imaging, we can diagnose thousands of conditions with precision. But is our obsession with labeling every symptom making us sicker instead of healthier? Dr. Suzanne O’Sullivan, an Irish neurologist and author of The Age of Diagnosis, argues that medicine has an over-diagnosis problem—and it’s causing real harm. Here’s what you need to know about this growing issue and how we can address it.
Over-diagnosis happens when a condition is correctly identified, but it would never have caused symptoms or harm if left undetected. Unlike misdiagnosis (a wrong diagnosis) or false positives (abnormal test results that turn out to be harmless), over-diagnosis involves a true medical condition that doesn’t need treatment. For example, advanced imaging might detect tiny, slow-growing cancers that would never progress, yet patients undergo stressful and risky treatments anyway.
O’Sullivan highlights startling statistics: autism diagnoses in the UK surged by 787% from 1998 to 2018, Lyme disease has an estimated 85% over-diagnosis rate in some regions, and cancer screening programs often detect abnormalities that don’t reduce death rates. These numbers suggest we’re labeling more people as “sick” without always improving their health.
Several factors drive this trend:
O’Sullivan also points to a psychological factor: the nocebo effect. Labeling someone with a diagnosis, even if it’s mild, can make them hyper-focused on their symptoms, worsening their mental and physical health. For example, telling a child they have mild autism might harm their self-esteem without providing clear benefits.
Over-diagnosis isn’t just a neutral label—it can hurt people in multiple ways:
O’Sullivan advocates for a “slow medicine” approach to counter over-diagnosis. This means:
O’Sullivan is clear: she’s not against medical advancements. Genetic testing for rare brain diseases, for instance, is a game-changer. But we need to balance these innovations with caution. Doctors should communicate the uncertainty of diagnoses, and patients should resist the urge to demand a label for every symptom. Policymakers, too, must address systemic drivers like overly broad disease definitions and financial incentives that fuel over-diagnosis.
Next time you’re at the doctor’s office, consider these steps to avoid over-diagnosis:
Integrative medicine providers combine conventional medical treatments with evidence-based complementary therapies, offering a holistic approach to healthcare. Here are key reasons to consider one:
Considerations: Not all therapies are covered by insurance, and costs can vary. Ensure the provider is licensed and uses evidence-based practices—check credentials through boards like the American Board of Integrative Medicine. If you’re dealing with a specific condition or seeking preventive care, they can tailor a plan, but discuss with your primary doctor to avoid treatment conflicts.
Medicine’s ability to diagnose has outpaced our ability to understand what those diagnoses mean. Over-diagnosis is a real problem, turning healthy people into patients and causing harm through stress, over treatment, and wasted resources.
By embracing “slow medicine” and fostering open conversations between doctors and patients, we can ensure diagnoses serve our health, not undermine it. As O’Sullivan puts it, sometimes less testing and diagnosing is the healthiest choice of all.
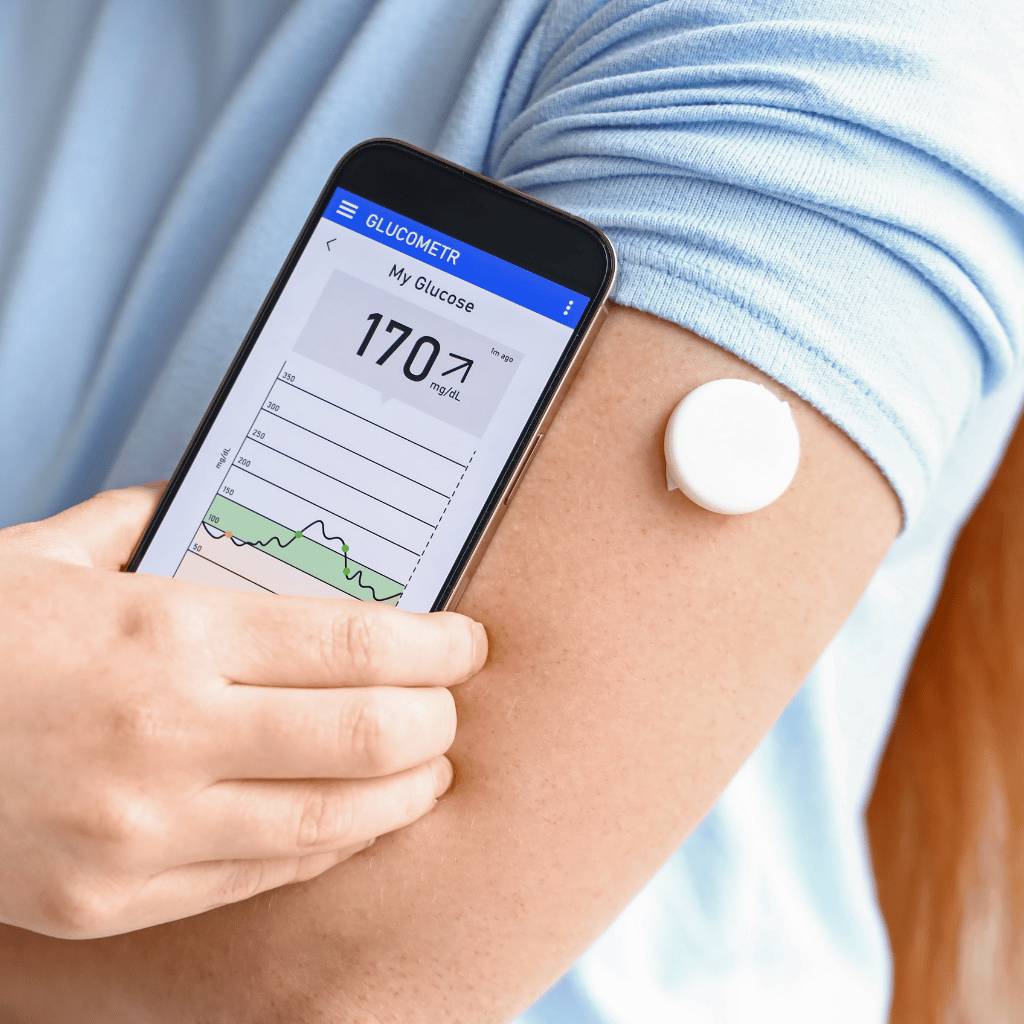
If you’ve been curious about how to keep a closer eye on your health without the hassle of constant finger pricks, let’s talk about continuous...

Have you ever wondered if your diet could hold the key to better health beyond quick fixes? AtHolistically Rx, we’re redefining wellness with...

When cardiologists jokingly suggested adding statins to the water supply to prevent heart attacks, it highlighted the transformative potential of a...